Effects of Relaxation Associated with Restricted Environmental Stimulation Therapy (REST) on Plasma Cortisol, ACTH, and LH
John W. Turner, Jr., and Thomas H. Fine
Medical College of Ohio
Restricted Environmental Stimulation Therapy (REST), which involves placing an individual into an environment of severely reduced stimulation for brief periods, has been subjectively reported to produce deep relaxation. The present study determines the effects of REST-assisted relaxation on plasma cortisol, ACTH, and luteinizing hormone (LH). These parameters were also measured in a group exposed to a similar relaxation paradigm, but without REST (non-REST). Each subject experienced two baseline sessions (1 and 2), four REST (or non-REST) relaxation sessions (3, 4, 5, 6), and two follow-up sessions (7and 8). Pre- and post-session plasma hormone levels were measured in sessions 1, 2, 5, and 8. Both REST and non-REST subjects reported that the experience was relaxing. During the treatment period (session 5) pre- to post-session changes in cortisol and A CTH, but not in LH, were significantly greater for the REST group than for the non-REST group. Plasma cortisol level also decreased across sessions in the REST group, with levels in sessions 5 and 8 significantly lower than the baseline (sessions I and 2). Non-Rest subjects showed no change in plasma cortisol across sessions. No significant change in plasma ACTH or LH occurred across sessions in the REST or non-REST groups, although ACTH showed a decreasing trend. These data demonstrate that repeated brief REST-assisted relaxation produces a relaxation state associated with specific decreases in pituitary-adrenal axis activity.
REST is the acronym for Restricted Environmental Stimulation Therapy. This procedure, which has previously been called sensory isolation or sensory deprivation (SD), involves placing an individual into an environment of severely reduced stimulation. Currently the two most frequently used REST methods are lying on a bed in a dark, soundproof room, and flotation in buoyant liquid at skin temperature in a light-free, soundproof chamber (Suedfeld, 1980). The flotation REST method, designed by Lilly (1977), produces a sense of profound relaxation as subjectively reported by numerous users of the method for brief (up to an hour) periods (Lilly, 1977). Physiological measures of subjects in classical SD studies frequently indicated increased arousal and sympathetic activity with isolation for 3 or more hours (reviewed by Zubeck, 1969; Selye, 1976; Zuckerman, Persky, Hopkins, Murtaugh, Basu, & Schilling, 1966; Mendelson, Kubzansky, Liederman, Wexler, Dutoit, & Solomon, 1960; Hanna, Burns, & Tiller, 1963). However, in studies of SD for 2 hours or less there were decreases observed in these parameters (reviewed by Zubeck, 1969; Hanna et al., 1963; Cohen, Silverman, & Shmavonian, 1962), suggesting a relaxation effect, and in a recent study in this laboratory repeated flotation REST-assisted relaxation resulted in clinically significant decreases in blood pressure in essential hypertensives (Fine & Turner, 1982). While the effect of stress on levels of adrenal-axis hormones are well documented (reviewed by Selye, 1976; Miyabo, Hisada, Asato, Mizushima, & Ueno, 1976), there have been few studies of relaxation effects on adrenal-axis activity, and results of these studies using various relaxation methodologies have been inconsistent. Davidson, Winchester, Taylor, Alderman, and Ingels (1979) reported decreased plasma norepinephrine in subjects given deep muscle relaxation training. However, relaxation associated with transcendental meditation had no effect on plasma norepinephrine and epinephrine (Michaels, Huber, & McCann, 1976). In other studies transcendental meditation was associated with variable effects on plasma cortisol (Jevning, Wilson, & Davidson, 1978; Jevning, Wilson, Vanderlaan & Levine, 1975; Michaels, Parra, McCann, & Vander, 1979). McGrady, Yonker, Tan, Fine, and Woerner (1981) reported that biofeedbackassisted relaxation resulted in decreased urinary cortisol but had no effect on plasma cortisol. We hypothesize that the particularly deep relaxation associated with REST could maximize the opportunity to observe hormonal changes in relaxation. The present study was undertaken to determine the effect of brief repeated flotation REST-assisted relaxation on plasma cortisol, ACTH, and luteinizing hormone in normal subjects.
Method
Subjects
Twelve normal white male volunteer subjects, aged 22-30, were studied. The subjects were recruited from a medical school class and were Hormones and Restricted Environmental Stimulation told that they were participating in a study of physiological changes associated with relaxation. All subjects were on a normal diet with normal mealtimes and normal sleep-wake cycles. Subjects were divided equally and randomly into two groups, one experiencing REST-assisted relaxation and one experiencing a similar relaxation procedure but without REST.
REST Chamber
Purchased from Samadhi Tank Company (Los Angeles), the chamber (#D6) was a rectangular box 8′ long, 4′ wide, and 42″ high, constructed of styrofoam backed with black plastic. Twenty-gauge vinyl (similar to that in a waterbed) lined the box and contained saturated Epsom salts solution (sp. gr. 1.3). Temperature control of the solution (94.0 _+ .5 ° F) was maintained through the use of a waterbed heater with a solid-state thermoregulator.
The REST chamber was completely enclosed, eliminating light. Marked sound attenuation (levels < l0 dB) occurred since the ears were submerged in the solution during flotation. These subjects floated nude in supine position with arms at their side. (see Figure 1).
REST-Assisted and Non-REST Relaxation Procedures
The REST procedure began with subjects in dim light in the chamber. The lights were decreased to complete darkness and the taped audio message “my arms and legs are heavy and warm” was played quietly for 90 seconds. Lights were then returned to baseline for 60 seconds while the subject allowed thoughts to flow without special focus (as per instruction). This procedure was repeated for 10 full cycles. Non-REST relaxation subjects were reclined in a reclining chair in a room with dim lights (< 1 ftcd) and little room noise (< 30 dB). These subjects received the same light-dark and message procedure as the REST group for l0 full cycles. The experiment was divided into three phases: baseline, REST or non-REST relaxation, and follow-up. Baseline was two sessions lasting 35 minutes each, with 1 day between the sessions. During baseline all subjects reclined quietly for 30 minutes in a reclining chair. Four days later REST sessions were begun. REST (or non-REST) relaxation was one 35-minute session per day as described above for 4 consecutive days. Four or 5 days later each subject had two 35-minute follow-up sessions in which they utilized their relaxation phrases in the same environment as for baseline. At the end of follow-up each subject was asked to fill out a brief questionnaire evaluating the relaxation experience. All sessions took place between 1200 and 1400 hr and all sessions for a given subject started within 1 hour of the same time each day. Blood samples were collected in heparinized vacutainers from the forearm, with subjects in a sitting position, before and after sessions l, 2, 5, and 8. Samples were centrifuged immediately and plasma was frozen. Cortisol was measured by radioimmunoassay (RIA) kit (Code KCOD2, Diagnostic Products, Los Angeles). ACTH was measured by RIA kit (Code IM66, Amersham Corporation, Chicago). Luteinizing hormone (LH) was measured by RIA kit (Code LM7011, Nichols Institute Diagnostics, San Pedro). Quality-control measures for each assay were within respective limits of acceptability. Assays were carried out in blind fashion. (Because several postsession blood samples were inadvertently destroyed, the Nis less than 6 in tables with prepost measures.) The results section is divided as follows: (1) cortisol, (2) ACTH and LH, and (3) attitudes of subjects. The hormone subsections are further subdivided according to the comparisons that were considered: (a) presession versus postsession for a given session (acute effects), (b) across sessions (long-term effects), i.e., baseline (sessions 1 and 2) versus treatment (session 5) versus follow-up (sessions 8), and (c) REST versus non-REST.
Hormones and Restricted Environmental Stimulation
Cortisol
Both pre- and postsession data are available for sessions 1, 5, and 8. Only presession data are available for session 2. Cortisol data were subjected to a repeated-measures ANOVA (2 X 2 X 3). The independent factors were as described above, (a) pre/post (within), (b) sessions (within), and (c) treatment (between). Significance for specific differences was determined by a Newman-Keuls multiple-range test.
Pre/Post.
In the REST – assisted group averaged postsession plasma cortisol levels were significantly (p < .05) lower than the presession levels in session 5 (treatment). Levels were not different in sessions 1 (baseline) or 8 (follow-up) (Table I). In the non-REST group average pre- and postsession plasma cortisol levels were not different for any session. In session 5 the REST-assisted group averaged 20.3o-/o pre- to postsession decrease, while the non-REST group averaged 7.3°70 decrease.
Across Sessions. Results presented in Figure 2 reflect pooled pre- and postsession values, since pre- and postsession measures showed significant interaction with across-session measures in ANOVA and the average values most effectively represent the long term. In the REST group plasma cortisol levels in the REST group were not different from levels in the non-REST group in sessions 1 and 2 but were lower than non-REST group levels in sessions 5 and 8 (p < .05).
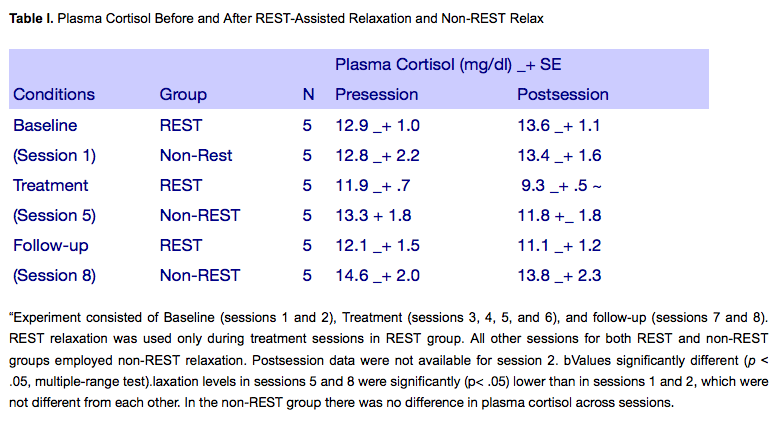
REST versus non-REST.
As shown in Figure 2, plasma cortisol levels in the REST group where not different from levels in the non-REST group in sessions 1 and 2 but were lower than non-REST group levels in sessions 5 and 8 (p<.05).
ACTH and LH
Due to variation in absolute ACTH and LH values among individuals, these data are presented in the form of postsession value as percent of presession value, which reflect pre to post changes. These data also did not meet basic criteria for parametric statistical analysis and therefore significance of specific differences was evaluated by nonparametric tests. Friedman test, Wilcoxon signed-rank test, and Mann-Whitney U test were appropriately employed.
Pre/Post.
No significant per/post differences in plasma LH occurred in any sessions, and no trends were apparent (Table II). Regarding plasma ACTH, a 39.3% decrease was observed in session 5 in the REST group.This decrease was significantly (p < .05, Wilcoxon test) greater than the decrease in session 1 in the rest group. No other significant pre/post changes occurred in any sessions in either the REST or non-REST group (Table II). Four of five subjects in the REST group showed a decrease in plasma ACTH in session 5, while four of five non-REST subjects showed no change or a slight increase in plasma ACTH in session 5.
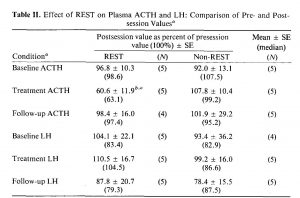
Across Sessions.
Plasma LH and ACTH levels in both the REST-assisted and non-REST relaxation group showed no differences across sessions.No trend was observed in plasma LH across sessions in either group. Average plasma ACTH levels showed a decreasing trend across sessions in the REST group but not in the non-REST group.
REST versus non-REST.
Regarding plasma LH no differences between REST and non-REST groups were observed in either pre/post or across-session measures. For ACTH the amount of change from pre- to postsession in the REST group was not different from that in the non-REST group in sessions 1 and 8. However, in session 5 the pre/post ACTH change in the REST group (39.3% decrease) was significantly (p < .05, Mann-Whitney U test) greater than in the non-REST group (3.9% decrease). As stated previously, in the REST group the pre/post differences in session 5 were significantly greater (p < .05, Wilcoxon test) than the respective pre/post differences in session 1. This comparison in the on-REST group showed no significant difference.
Summary.
Plasma cortisol and ACTH, but not plasma LH, showed significant changes. Both cortisol and ACTH decreased only in the REST group and only in session 5 in that group. Plasma cortisol, but not ACTH or LH, showed a decrease across sessions in the REST group only, being lower in both treatment and follow-up than in baseline. ACTH, but not LH, showed a decreasing trend across sessions.
Attitudes of Subjects.
At the end of follow-up, all subjects were asked to rate the following questions on a 0-to-5 scale: (a) Do you believe you learned a relaxation technique? (b) Did you experience physical relaxation during the procedure? (c) Did you experience mental relaxation during the procedure? All REST subjects and all except one non-REST subject responded to question (a) at a 4 or 5 rating and to question (b) at a 5 rating. The average rating for question (c) was slightly higher for REST (4.8) than for non-REST (4.0) subject, and this difference was significant (p < .05), t test).
Discussion
The repeated REST-assisted relaxation sessions in this study were associated with a significant decrease in plasma cortisol across sessions. This suggestion of decreased adrenal-axis activity is consistent with the verbal reports of the REST subjects, each of whom found the experience “very relaxing.” The REST effect on plasma cortisol appears to be due to more than the use of a relaxation procedure alone, since subjects exposed to a similar relaxation paradigm (non-REST relaxation) showed no change in plasma cortisol. It may be noteworthy that although REST and non-REST groups reported equivalent physical relaxation, the REST group reported greater mental relaxation than the controls. The REST-assisted relaxation sessions in this study were not continuous sensory isolation, since autogenic phrases and dim light were inserted at repeated intervals during the sessions. However, sensory input was greatly attenuated.
Although the data for ACTH is less clear than for cortisol, it appears that less ACTH was released during sessions 5 (treatment) in the REST group than in the non-REST group. In addition, it appears that relatively less ACTH was secreted in sessions 5 than in baseline. As with cortisol data, these data are consistent with the concept of decreased adrenal-axis activity associated with REST. The fact that plasma ACTH did change and plasma LH did not change during REST-assisted relaxation suggests that the endocrine response to REST-assisted relaxation at the pituitary level may represent a specific action of the adrenal axis rather than a general decrease in pituitary activity.
Both LH and ACTH values varied considerably within and among subjects, and cortisol showed some variation among subjects. In view of the reasonably short circulating half-life of ACTH (Besser, Orth, Nicholson, Byyny, Abe, & Woodham, 1971) and LH (Schalch, Parlow, Boon, & Reichlin, 1968) and the pulsatile release patterns that have been demonstrated for these hormones (Boyar, Perlow, Hellman, Kapen, & Weitzman, 1972; Gallagher, Yoshida, Roffwarg, Fukushima, Weitzman, & Hellamn, 1973; Filicori, Bolelli, Franceschetti, & Lafisca, 1979), it is probable that consistent values cannot be obtained using single samples. It appears that long-term single-subject studies would be advantageous, andfor protein hormone measurement at least, three closely spaced bloodsamples per data point should be used. This approach would minimize variability that might mask the relatively small changes in basal hormone levels associated with relaxation.
A surprising finding in this study was that plasma cortisol levels, which did show consistent decreases across REST subjects, were still below baseline in the follow-up period, which was 4-5 days after REST sessions had ended. The reason for this is unknown. It is possible that REST-assisted relaxation may exert a carry-over effect on the regulation of plasma cortisol. It has been demonstrated that biofeedback-assisted relaxation training can lead to a physiological change such as blood pressure reduction that is maintained well beyond the training sessions (Patel, 1975; Patel & North, 1975). Since the decrease in cortisol across sessions was not associated with a significant across-session decrease in ACTH, no cause-effect relationship can be established. However, ACTH did show a decreasing trend across sessions, and it may be that the variability in ACTH values precluded observation of a significant effect. The observance of significantly greater decreases in plasma cortisol within the REST treatment session as compared to baseline or non-REST relaxation suggests a specific effect of REST on cortisol release or removal from the circulation. It seems certain that release was affected, since plasma ACTH was also decreased during the REST treatment session (see Table II). The 20% decrease in plasma cortisol during a 35-minute REST session in the present study is similar to the 260?0 decrease in plasma cortisol in 30 minutes of transcendental meditation (TH) reported by Jevning et al. (1978). It is noteworthy that the present study employed naive subjects, while the TM study used regularly practicing meditators with 3-5 years’ experience, Michaels et al. (1979) found no decrease in plasma cortisol associated with 20-30 minutes of TM in regularly practicing meditators with at least 2 years’ experience. Similarly conflicting results have been obtained in acrosssession studies of EMG biofeedback-assisted relaxation and cortisol in hypertensive subjects. McGrady, Tan, Crane, Fine, and Yonker (1979)found no effect of 16 30-minute biofeedback sessions on plasma cortisol, but they observed decreased urinary cortisol in a separate study (McGrady et al., 1981) using similar protocol. In the present study naive subjects reported experiencing deep relaxation and showed statistically significant decreases in adrenal-axis activity after three REST sessions. In most forms of relaxation such as transcendental meditation or biofeedback-assisted relaxation the individual must elicit relaxation by utilizing some internal strategy. In contrast, REST-assisted relaxation utilizes the environment to induce relaxation with the individual passively experiencing the process. The effortless passive relaxation of REST may provide an advantage over methods requiring a trial-and-error approach to the deep relaxation state. All the changes observed in the hormone levels in this study were within the limits of what is routinely accepted in radioimmunoassay as “normal.” However, cortisol has a number of target tissues and has demonstrable effects on physiological functions such as metabolism, the immune response, and neural homeostasis. The possible long-term effects of small but persistent changes in plasma cortisol levels within this “normal” range are unknown, at both the tissue and the whole individual level. Furthermore, although the ability of behavior to modify physiology is well documented in biofeedback, the possible mediation of such phenomena by hormones has received little attention. It is interesting to consider, for example, that the conditioned learning of immunosuppression in rats demonstrated by Ader and Cohen (1975) may in part be mediated by small, long-term changes in plasma ACTH and cortisol within the “normal” range. The results of the present study offer incentive for continued investigation of the relationship between endocrine patterns and behavioural state in the individual utilizing the REST approach.
REFERENCES
- Ader, R., & Cohen, N. Behaviorally conditioned immunosuppression.Psychosomatic Medicine. 1975, 37,333-340
- Besser, G. M., Orth, D. N., Nicholson, W. E., Byyny, R. L., Abe, K., & Woodham, J. P. Dissociation of the disappearance of bioactive and radioimmunoactive ACTH from plasma in man. 595-603.
- Boyar, R., Perlow, M., Hellman, L., Kapen, S., & Weitzman, E. Twenty-four hour pattern of luteinizing hormone secretion in normal men with sleep stage recording.of Clinical Endocrinology and Metabolism, 1972, 35. 72-81. 1972, 35, 72-81.
- Cohen, S. I., Silverman, A. J., & Shmavonia, B. M. Psychophysiological studies in altered sensory environments. Journal of Psyehosomatic Research, 1962, 6, 259-281.
- Davidson, D. M., Winchester, M. A., Taylor, C. B., Alderman, E. A., & Ingels, N. B. Effects of relaxation therapy on cardiac performance and sympathetic activity in patients with organic heart disease. Psychosomatic Medicine, 1979, 41, 303-309.
- Filicori, M., Bolelli, G., Franceschetti, F., & Lafisca, S. The ultraradian pulsatile release of gonadotropins in normal female subjects. ACTA European Fertility, 1979, 10(1), 29-33.
- Fine, T. H., & Turner, J. W., Jr. The effect of brief restricted environmental stimulation therapy in the treatment of essential hypertension.
- Behavioral Therapist, 1982, 520: 567-570.
- Gallagher, T. F., Yoshida, K., Roffwarg, H. Fukushima, D., Weitzman, E., & Hellman, L. ACTH and cortisol secretory patterns in man. Journal of Clinical Endocrinology and Metabolism, 1973, 36, 1058-1068.
- Hanna, T. D., BurnscN. M., & Tiller, P. R. Behavioral and physiological response to varying periods of sensory deprivation. Air Crew Equipment Laboratory, U.S. Naval Air Material Center, Philadelphia, Bureau of Medicine Subtask, 1963, MR005, 13-066.6.
- Jevning, R., Wilson, A., & Davidson, J. M. Adrenocortical activity during meditation. Hormones and Behavior, 1978, 10, 54-60.
- Jevning, R., Wilson, A., Vanderlaan, E., & Levine, S. Plasma prolactin and cortisol during transcendental meditation. Proceedings of the Endocrine Society, 1975, p. 257.
- Lilly, J. C. The deep self. New York: Simon & Schuster, 1977.
- McGrady, A. V., Tan, S. V., Crane, R. Fine, T., & Yonker, R. Biochemical correlates ofbiofeedback in essential hypertension. Biofeedback and Self-Regulation, 1979, 4, 258.
- McGrady, A. V., Yonker, R., Tan, S. Y., Fine, T. H., & Woerner, M. The effect of biofeedback assisted relaxation training on blood pressure and selected biochemical parameters in patients with essential hypertension. Biofeedback and Self-Regulation, 1981, 6, 343-353.
- Mendelson, J., Kubzansky, P. E., Liederman, P. H., Wexler, D., Dutoit, D., & Solomon, P. Cathecholamine excretion and behavior during sensory deprivation. Archives of General Psychiatry, 1960, 116, 883-888.
- Michaels, R. R., Huber, M. J., & McCann, D. S. Evaluation of transcendental meditation as a method of reducing stress. Science, 1976, 192, 1242-1244.
- Michaels, R. R., Parra, J., McCann, D. S., & Vander, A. J. Renin. Cortisol and aldosterone during transcendental meditation. Psychosomatic Medicine, 1979, 41, 50-54.
- Miyabo, S., Hisada, T., Asato, T., Mizushima, N., & Ueno, K. Growth hormone and cortisol responses to psychological stress: Comparison of normal and neurotic subjects. Journal of Clinical Endocrinology and Metabolism, 1976, 42, 1116-1120.
- Patel, C. Twelve-month follow-up of yoga and biofeedback in the management of hypertension. Lancet, 1975, 1, 62-65.
- Patel, C. H., & North, W. R. S. Randomized controlled trial of yoga and biofeedback in management of hypertension. Lancet, 1975, 2, 93-95.
- Schalch, D. S., Parlow, A. F., Boon, R. C., & Reichlin, S. J. Measurement of human luteinizing hormone in plasma by radioimmunoassay. Journal of Clinical Investigators, 1968, 47, 665-678.
- Selye, H. Stress in health and disease. Boston: Butterworths, 1976, 1256 p.
- Suedfeld, P. In Restricted environmental stimulation: Research and clinical applications. New York: Wiley, 1980.
- Zubeck, J. P. In J. Zubeck (Ed.), Sensory deprivation: Fifteen years of research. Appleton-Century-Crofts, 1969. Pp. 254-289.
- Zuckerman, M. Persky, H., Hopkins, T. R., Murtaugh, T., Basu, G. K., & Schilling, M. Comparison of stress effects of

